Adapted from an original article by Joel Guarna at contextualscience.org
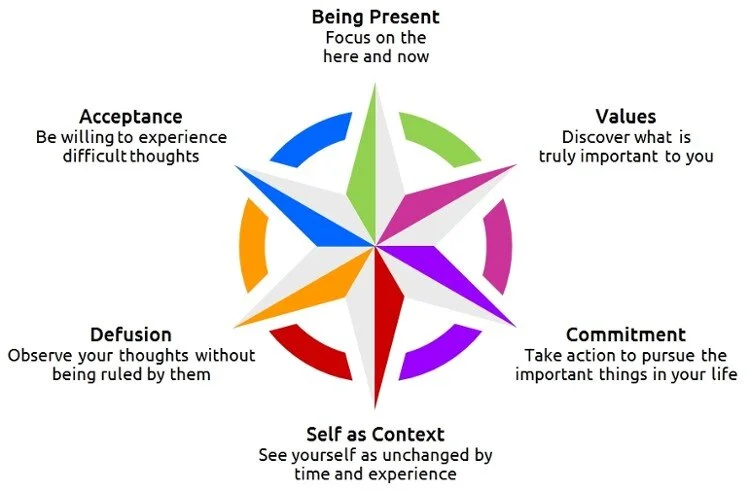
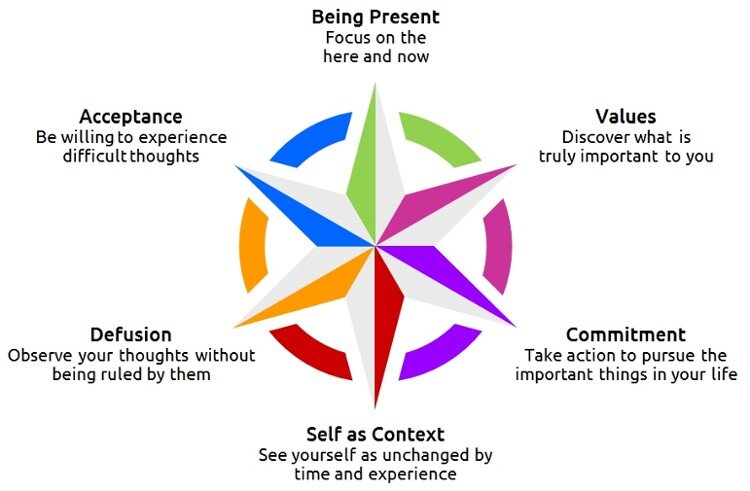
What is Acceptance and Commitment Therapy (ACT, said as the word "act")? ACT, just approaching its 30th anniversary since its inception, is an innovative form of behavioral and cognitive therapy that has built upon both the strengths and the weaknesses of traditional cognitive-behavioral therapy (CBT).
CBT has become the most well-known, mainstream approach to therapy, partly because it has, by far, the strongest research support for its effectiveness in treating a wide range of emotional and behavioral problems. CBT has been found effective in treating depression, anxiety disorders, the effects of trauma, substance abuse and addiction, complications related to medical conditions, and many other conditions.
ACT is based on a behavioral account of human language and cognition called Relational Frame Theory (RFT) which has generated research into human language and cognition, providing fuel for the development of new treatment approaches. The "fruit" of this progress can be found in the philosophy and basic concepts underlying ACT. ACT has moved away from the traditional CBT emphasis on changing or correcting one's thoughts in order to alleviate suffering. Instead, ACT aims to alter the functions of our private experiences (thoughts, feelings, memories, bodily reactions), so they no longer entangle us. Said another way, ACT aims to change our relationship with these private events so we can become free from their grip, and free from the patterns that bind us and prevent us from living a flexible, meaningful, and enjoyable life. In the service of these aims, ACT incorporates acceptance strategies, mindfulness techniques, and a wide range of behavioral approaches already known to be effective from CBT.
ACT is one of a family of interventions inside the CBT tradition writ large that are focusing on the person's relationship to experiences rather than on the content of these experiences. The data on ACT and related approaches are moving CBT itself toward a new model that emphasizes being open, centered, mindful and actively pursuing values. Because of that, ACT and CBT as a larger tradition are becoming more difficult to distinguish over time.
At Better Health Psychology, when we meet you, we tailor your therapy to treat your specific problem. We use a variety of therapies, including CBT and ACT therapies, and take the best parts of these therapies that are most useful and suitable to help you to achieve your treatment goals.
Hypervigilance: What you need to know
Original Source is from an article by Lana Burgess in Medical News Today, 7th Sept 2017
What is hypervigilance?
Hypervigilance is a state of heightened alertness accompanied by behaviour that aims to prevent danger. But what are its main symptoms and how can it be treated?
Understanding hypervigilance can enable people to access the right sort of help and better manage their symptoms. This article explores the symptoms, causes, and treatments for hypervigilance.
Having their senses on high alert means that people with hypervigilance often feel there is a threat close by.
People experiencing hypervigilance are unusually sensitive to the environment and people around them.
It is not a condition in itself, but a way of behaving that may be caused by trauma or an underlying mental health problem.
When someone experiences hypervigilance, their subconscious is constantly anticipating danger. As a result, their senses are on high alert, ready to spot and respond to any danger.
The situations they are trying to spot might be:
a physical danger
a repeat of a traumatic event
something wrong in a relationship
This super alertness makes people with hypervigilance feel and act as though there is always a threat around the corner.
Normally, they are not responding to a real threat. Rather, their brain is overanalysing, and overreacting to, input from their senses.
Hypervigilance can be a symptom of:
post-traumatic stress disorder (PTSD)
anxiety
other mental health conditions
Hypervigilance vs. paranoia
The way people behave when they are experiencing hypervigilance can seem similar to paranoia. However, there are important differences between the two mental states:
Delusion vs. being on guard: In paranoia, people hold specific, untrue beliefs that certain people or things are out to get them. People experiencing hypervigilance do not have any fixed beliefs about a specific thing happening, however. They are not delusional but just on high alert.
Now vs. in the future: In paranoia, people have a delusional belief that someone or something is trying to harm them now, in the present. In hypervigilance, people are on guard in anticipation of something bad happening in the future.
Lack of awareness vs. insight: In paranoia, people will not be aware that they are suffering from an illness and may believe that their delusions are true. In hypervigilance, people often have an awareness that there is no objective reason to be on edge, but find it hard to relax nonetheless.
Symptoms
There are some physical symptoms of hypervigilance, but most symptoms are behavioural. The physical signs and behaviours that people experiencing hypervigilance may show are explored below.
Physical symptoms
Some physical symptoms of hypervigilance include sweating, quick breathing, and dilated pupils.
Not everyone experiencing hypervigilance shows physical signs, but some do.
When people do show physical symptoms, they may include:
dilated pupils
breathing very quickly
seeming restless
sweating
having a rapid heart beat
Behavioural symptoms
The way a person behaves when they are experiencing hypervigilance can vary. However, there are some common types of behaviour that often occur.
People experiencing hypervigilance may:
keep checking their surroundings and find it hard to focus on conversations
be easily startled and jump or scream at things they hear or see suddenly
overreact to things happening around them in a way that may seem hostile
find crowded or noisy environments overwhelming
look closely at people to see if they are holding weapons
overanalyse situations and believe them to be worse than they are
overestimate the chances of a bad thing happening to them physically or in their relationships
be overly sensitive to people's tone or expressions, taking them personally
have trouble getting to sleep or staying asleep
Complications
Due to the way hypervigilance may cause people to behave, there can be some long-term complications. These include:
obsessive behaviour patterns
physical and mental exhaustion
difficulty in relationships
problems in the workplace
avoidance of social situations
Causes
Hypervigilance is the brain's way of protecting the body from danger. As such, people fighting in the military or experiencing violence at home may exhibit hypervigilance with good reason.
However, hypervigilance can also happen when there is not a real, physical danger. When this happens, it is as a result of a mental health condition.
Mental health conditions that can cause hypervigilance include:
PTSD
PTSD is an anxiety disorder that people can develop after experiencing or seeing a traumatic or life-threatening event. Events that can cause PTSD include:
military combat
death of a loved one
sexual assault
serious accidents
prolonged bullying
Hypervigilance is a key feature of PTSD, as people are in fear of re-living the trauma. This can cause them to be constantly on-guard, in anticipation of the trauma happening again.
Anxiety
People diagnosed with generalized anxiety disorder (GAD) or social anxiety may experience hypervigilance. This is most likely to happen in new situations or when they meet new people.
However, there is some debate as to whether anxiety causes hypervigilance, or whether anxiety disorders result from hyper vigilant behaviour. More research is needed to understand whether hypervigilance is a symptom or a cause of anxiety disorders.
Other mental health conditions
Hypervigilance may also occur in people with other mental health conditions. These may include:
schizophrenia
obsessive-compulsive disorder
bipolar disorder
Triggers
Hypervigilant behaviour may be triggered by crowded environments, uncertain situations, and feelings of claustrophobia.
There are common triggers that can bring on hypervigilant behaviour in those who are affected by it. These triggers include:
feeling claustrophobic
crowded environments
uncertain situations
reminders of past trauma
arguments and shouting
criticism or embarrassment
competing demands or expectations
chaotic behaviour by others
feeling as if they have been abandoned
feeling or anticipating pain
being emotionally distressed
Treatment
The first step in treatment if a person experiences hypervigilance due to domestic violence or military combat, is to remove them from the dangerous environment.
When someone experiences hypervigilance due to a mental health condition, other treatments that may help include:
Therapy: A doctor may refer people for therapy to help treat the mental health condition that is causing their hypervigilance. Therapies that may help include cognitive behavioural therapy (CBT) for anxiety or exposure therapy for PTSD.
Medication: Anxiety and PTSD can be treated with beta-blockers, antidepressant, or anti-anxiety medication. Schizophrenia or bipolar may be treated with antipsychotics.
Management techniques
As well as taking medication if it is prescribed and attending therapy if they have been referred, people may look for other ways to manage hypervigilance.
The following techniques are among those that can help:
Relaxation: Deep breathing exercises or yoga may aid relaxation and help reduce anxiety so that people can better manage their symptoms.
Exercise: Regular will release endorphins, which may help reduce anxiety.
Mindfulness: Being mindful of how they are feeling and focusing on the moment may help people monitor and reduce their hypervigilant behaviour.
Communication: Expressing how they are feeling to others and being willing to accept feedback about times they may have overreacted can be helpful.
Objectivity: Looking for objective evidence, as to whether there is a need to be so on guard, may help people monitor their hypervigilant behaviour.